Report to: Board of Health
Meeting Date: February 3, 2016
Report Number: BOH Report – BH.01.FEB0316.R02
Prepared by: Katherine Paphitis, Public Health Inspector (CID) Janice Walters, Manager, Control of Infectious Diseases
Approved by: Rob Thompson, Director, Health Protection
Submitted by: Dr. Nicola Mercer, Medical Officer of Health & CEO
Recommendation(s)
(a) That the Board of Health receives this report for information
EXECUTIVE SUMMARY
Wellington-Dufferin-Guelph Public Health (WDGPH) is responsible for the investigation and management of enteric and respiratory outbreaks in institutions.1 Institutions include retirement homes (RH), long-term care homes (LTCH), licensed daycares, group homes and hospitals. Institutional outbreak management often requires a significant amount of Public Health involvement. The degree of involvement depends on the type of outbreak, the type of facility and how well the facility is able to implement and comply with recommended infection control measures.
The Ministry of Health and Long-Term Care (MOHLTC) has created Best Practice documents to assist facilities in recognizing and managing both respiratory and enteric outbreaks.2,3 These documents outline the criteria needed to define a suspected or confirmed outbreak of illness and provide guidance around the control measures needed to minimize transmission within the facility and end the outbreak.
During 2015, WDGPH reported a total of 156 unique outbreaks to the MOHLTC via the integrated Public Health Information System (iPHIS). Of these 156 outbreaks; 14 ultimately did not meet the definition of a confirmed or suspect outbreak, 14 were created for the purpose of mandatory aggregate chickenpox reporting to the MOHLTC, one represented a Clostridium difficile infection (CDI) outbreak in an area hospital and two were true community outbreaks involving mumps and hepatitis A respectively. The remaining 125 reported outbreaks were confirmed or suspected enteric (n=63) or respiratory (n=62) outbreaks in institutional settings.
Outbreak duration is defined in this report as the period from the onset of symptoms in the index case to the date on which the outbreak was declared over. Institutional respiratory outbreaks had a range of duration of five to 49 days with a median of 15 days and an average of 16 days. Institutional enteric outbreaks had a range of duration of four to 47 days with a median of 14 days and an average of 16 days. Note that three respiratory and one enteric institutional outbreaks were not included in the duration calculations as these outbreaks were still ongoing at the time of this report.
BACKGROUND
The timely identification of outbreaks and subsequent outbreak response by Public Health is important in controlling the spread of infectious disease within WDGPH. Outbreaks represent an opportunity for Public Health staff to work collaboratively with area institutions and to provide information and messaging on current infection prevention and control recommendations and best practices.
Public Health’s response to and involvement in the management of a suspected or confirmed facility outbreak typically involves the following actions:
- Confirming and monitoring the control of an outbreak, including the daily review of line listings (line lists outline the number of resident/child and staff cases, dates of illness onset and resolution, symptoms and complications).
- Creating an outbreak number and reporting the outbreak to the MOHLTC via iPHIS.
- Notifying the Public Health Ontario Laboratory (PHOL) of all confirmed and suspected outbreaks with specimens pending.
- Reviewing the facility’s infection prevention and control practices, including but not limited to assessment of housekeeping practices, type and use of disinfectants available on site, staff immunization rates for influenza, initiation of isolation of symptomatic residents and staff exclusion and cohorting (limiting staff movement within the facility).
- Performing a site inspection of the affected facility to ensure outbreak signage is posted, confirming the use of appropriate personal protection equipment, providing specimen kits (for facilities to collect stool/nasopharyngeal swabs from affected individuals with a goal of identifying a causative agent) and conducting an inspection/audit (to identify any potential infection control lapses, and in the case of an outbreak of gastroenteritis, to rule out food prepared onsite as the potential cause of illness).
- Attending outbreak meetings with facility department heads.
- Participating in daily facility communications in order to provide infection control recommendations and remain informed as to the status of the outbreak.
- Facilitating the collection and submission of specimens to the PHOL.
- Maintaining documentation in the electronic health record (EHR) and iPHIS regarding outbreak communications, updating of line lists, hospitalization and deaths and all actions and control measures recommended by Public Health.
- Reviewing literature in order to support any new infection control recommendations.
- Performing case by case assessment of repatriation requests, working with the facility and local community partners in order to determine whether a client may be returned or admitted to a facility or transferred between facilities, including hospitals, during the outbreak.
- Providing direction on any activities that must be postponed, cancelled or modified while the outbreak is ongoing.
- Distributing updated outbreak bulletins to community partners regarding outbreaks in LTCHs, RHs and hospitals.
- Preparing an outbreak summary report at the conclusion of the outbreak in order to identify any actions that may be improved upon in future outbreaks, and to highlight any outbreak control activities the facility did well, with a goal of preventing future outbreaks.
- Working with community partners who provide care in the outbreak facility to ensure appropriate processes are followed.
- Closing the outbreak in iPHIS and Excelicare (the EHR).
ANALYSIS/RATIONALE
The 156 unique outbreaks reported by WDGPH to the MOHLTC in 2015 represent a significant increase over both 2014 (n=115) and 2013 (n=124). Table 1 compares outbreak types by calendar year, from 2013 to 2015.
|
Outbreak Type* |
Number of outbreaks reported | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| CDI – Hospital | 1 | 0 | 2 |
| Chickenpox** | 14 | 11 | 13 |
| Community – Enteric | 1 | 2 | 7 |
| Community – Respiratory | 1 | 1 | 0 |
| Institutional – Enteric | 64 | 50 | 50 |
| Institutional – Respiratory | 75 | 51 | 52 |
| 156 | 115 | 124 | |
*Including outbreak classifications of “confirmed”, “suspect” and “does not meet outbreak definition”
**Created as outbreaks for the purpose of MOHLTC monthly aggregate reporting
Sporadic cases of chickenpox are created as outbreaks in iPHIS for the purpose of monthly aggregate case reporting to the MOHLTC and are excluded from the remainder of this report (n=14). In 2015 there was also one Clostridium difficile infection (CDI) hospital outbreak, one community mumps outbreak and one community hepatitis A outbreak. These three outbreaks and the 14 enteric and respiratory institutional outbreaks that did not meet case definition are excluded from further analyses. The number of confirmed or suspected outbreaks in institutions (n=125) are reported in Table 2.
| Facility Type | Number of Institutional and Respiratory Outbreaks Reported | ||
|---|---|---|---|
| Enteric Outbreaks | Respiratory Outbreaks | Total | |
| LTC/RH | 30 | 56 | 86 |
| Hospital | 3 | 6 | 9 |
| Daycare | 29 | N/A | 29 |
| Group Home | 1 | 0 | 1 |
| Total | 63 | 62 | 125 |
All institutional respiratory and enteric outbreaks reported in 2015 with a classification of “confirmed” or “suspect” (n=125) are summarized by month in Figure 1.
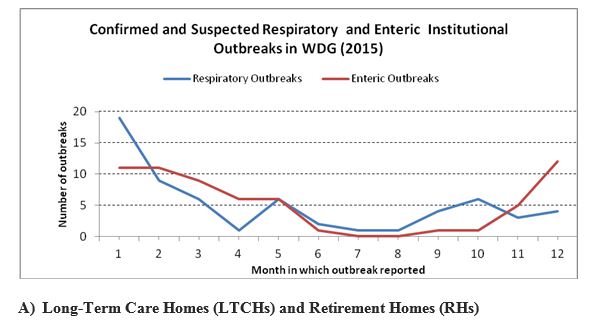
Data Table for line graph image:
| Month | Number of Respiratory Outbreaks | Number of Enteric Outbreaks |
|---|---|---|
| 1 | 19 | 11 |
| 2 | 9 | 11 |
| 3 | 6 | 9 |
| 4 | 1 | 6 |
| 5 | 6 | 6 |
| 6 | 2 | 1 |
| 7 | 1 | 0 |
| 8 | 1 | 0 |
| 9 | 4 | 1 |
| 10 | 6 | 1 |
| 11 | 3 | 5 |
| 12 | 4 | 12 |
Respiratory Outbreaks in Area RHs and LTCHs
In 2015, WDGPH received reports of 56 confirmed or suspected respiratory outbreaks in area RHs and LTCH, a 37% increase over the previous year (2014) in which 41 respiratory outbreaks were reported. Many factors influence the number of outbreaks that occur each year, including whether or not the seasonal influenza vaccine is a good match to circulating disease strains and whether uptake of the vaccine among institutionalized clients, facility staff members and members of the public is sufficient in order to minimize the spread of disease. In 2015 the 2014/2015 seasonal influenza vaccine was not a good match to circulating strains of Influenza A(H3N2), the dominant circulating strain.4 Influenza A virus was isolated in 21 of the respiratory outbreaks reported to WDGPH in 2015, whereas influenza B was only isolated in a single outbreak. A total of 15 outbreaks were classified as respiratory infection unspecified or unknown either due to a lack of specimens being submitted to the PHOL during the outbreak or due to no organism being identified during testing. Table 3 summarizes respiratory institutional outbreaks by the identified organism (if applicable) reported from 2013- 2015.
| Identified Organism | Number of outbreaks where organism identified | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| Influenza A | 21 | 12 | 13 |
| Influenza B | 1 | 7 | 2 |
| Rhinovirus | 8 | 8 | 8 |
| Coronavirus | 4 | 2 | 1 |
| RSV | 3 | 5 | 5 |
| Entero/Rhinovirus | 2 | 0 | 1 |
| Unspecified/unknown | 15 | 4 | 7 |
| Adenovirus | 0 | 1 | 0 |
| Metapneumovirus | 0 | 1 | 5 |
| Parainfluenza Virus | 0 | 1 | 4 |
| Coronavirus/Parainfluenza virus | 1 | 0 | 0 |
| 56 | 41 | 46 | |
Duration of Respiratory Outbreaks in RHs and LTCHs
The duration of the respiratory outbreaks (all types) ranged from five to 49 days, with a median of 15 days and a mean (average) of 16 days. The duration of the influenza outbreaks ranged from eight to 49 days, with a median of 15 days and an average of 17 days.
Enteric Outbreaks in Area RHs and LTCs
In 2015, WDGPH received reports of 30 confirmed or suspected enteric outbreaks in area RHs and LTCHs, a 7% increase from the previous year, in which 28 outbreaks were reported. 12 of the enteric outbreaks in 2015 were norovirus outbreaks while the other 18 were recorded as unknown or unspecified gastroenteritis. Table 4 summarizes the enteric institutional outbreaks by the identified organism (if applicable) from 2013-2015.
| Identified Organism | Number of outbreaks where organism identified | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| Norovirus | 12 | 11 | 13 |
| Gastroenteritis unspecified/unknown | 18 | 17 | 8 |
| Clostridium difficile | 0 | 0 | 1 |
| Rotavirus | 0 | 0 | 3 |
| Calicivirus | 0 | 0 | 1 |
| 30 | 28 | 26 | |
Duration of Enteric Outbreaks in RHs and LTCHs
The duration of the enteric outbreaks ranged from four to 39 days with a median of 14 days and an average of 15 days.
B.) Licensed Child Care Facilities (Daycares)
Respiratory Outbreaks in Daycares
WDGPH does not declare respiratory outbreaks in daycares unless an unusual reportable organism (e.g., pertussis) is confirmed to be the cause of an observed increase in respiratory illness within the centre.
Enteric Outbreaks in Daycares
WDGPH does manage enteric outbreaks in daycares. Initially, Public Health investigates to ensure the enteric outbreak is not related to food safety and/or a food borne pathogen. 29 enteric outbreaks were reported to WDGPH in area daycares in 2015. This represented a 53% increase from the previous year in which 19 outbreaks were reported. Norovirus was identified in two of the enteric outbreaks reported in 2015, with the remainder classified as gastroenteritis unspecified or unknown. Table 5 summarizes enteric outbreaks reported in daycares from 2013-2015.
| Identified Organism | Number of outbreaks where organism identified | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| Norovirus | 2 | 2 | 4 |
| Gastroenteritis unspecified/unknown | 27 | 17 | 19 |
| 29 | 19 | 23 | |
Duration of Enteric Outbreaks in Daycares
The duration of enteric outbreaks reported to WDGPH by area daycares in 2015 ranged from nine to 47 days with a median of 14 days and an average of 17 days.
C.) Hospitals
Respiratory Outbreaks in Hospitals
In 2015, there were six respiratory outbreaks reported to WDGPH by area hospitals, an increase from the previous two years in which no outbreaks (2014) and three outbreaks (2013) were reported (Table 6). Influenza A was isolated in two of these outbreaks and influenza B was isolated in the remaining four outbreaks. Both influenza A outbreaks were further characterized as influenza A, subtype H3.
Duration of Respiratory Outbreaks in Hospitals
The duration of respiratory outbreaks reported to WDGPH by hospitals in 2015 ranged from seven to 42 days with a median of 11 days and an average of 16 days.
| Identified Organism | Number of outbreaks where organism identified | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| Influenza A | 2 | 0 | 2 |
| Influenza B | 4 | 0 | 1 |
| 6 | 0 | 3 | |
Enteric Outbreaks in Hospitals
In 2015, there were three enteric outbreaks reported to WDGPH by area hospitals. This represented an increase from the previous two years in which no outbreaks (2014) and two outbreaks (2013) were reported. No organisms were identified in any of these outbreaks (Table 7).
Duration of Enteric Outbreaks in Hospitals
The duration of enteric outbreaks reported to WDGPH by area hospitals in 2015 ranged from eight to 14 days with a median of ten days and an average of 11 days.
| Identified Organism | Number of outbreaks where organism identified | ||
|---|---|---|---|
| 2015 | 2014 | 2013 | |
| Gastroenteritis unspecified | 3 | 0 | 2 |
| 3 | 0 | 2 | |
D.) Group Homes
In 2015, there was a single enteric outbreak reported to WDGPH in a group home. Norovirus was identified during this outbreak, which lasted a total of ten days.
The Public Health management of institutional outbreaks is becoming an increasingly challenging responsibility as LTCHs and RHs provide care to an increasing number of acute and complex residents, have difficulty retaining long-term employees and have limited human resources/time for infection control and outbreak management. Similarly, hospitals have a constant demand for beds and routinely request transfers and repatriations of patients to LTCHs and RHs in a declared outbreak. Best practice documents set out criteria for outbreak management and discourage repatriation of non line-listed (well) residents during an outbreak. The longest outbreak in 2015 lasted a total of 49 days; outbreaks of prolonged duration can have a significant negative impact on both residents and facilities requiring repatriation if these requests are not able to be approved or accommodated while the outbreak is ongoing. Public Health’s goal is to build infection control capacity in institutions while balancing the urgent bed needs of hospitals with the potential risk/benefit of the transfer to the vulnerable resident.
Ontario Public Health Standards
The goal of the Infectious Diseases Prevention and Control Standard is to prevent or reduce the burden of infectious disease of public health importance.1
Under the current Public Health Infectious Diseases Program Standards, Requirement #8 states, public health units are required to ‘provide public health management of cases and outbreaks to minimize the public health risk in accordance with the Infectious Diseases Protocol, 2008 (or as current); the Institutional/Facility Outbreak Prevention and Control Protocol, 2008 (or as current); and provincial and national protocols on best practices.’1
Additionally, under Requirement #7 of this Standard, ‘a medical officer of health or designate (must be) available on a 24/7 basis to receive reports of and respond to (outbreaks and) infectious diseases of public health importance…’.1 To comply with this requirement, a member of the Health Protection Division along with an agency program manager or director is always on-call after hours, weekends, and holidays in order to respond to reports in a timely manner. Institutions which are required to report suspected or confirmed outbreaks include long-term care homes (LTCH), licensed daycare centres, hospitals, and other institutional settings3.
Public Health units have additional responsibilities under the Institutional/Facility Outbreak Prevention and Control Protocol, 2015 and the Infection Prevention and Control in Licensed Day Nurseries Protocol, 2008 which include actions to detect and manage outbreaks, as well as to prevent the occurrence of future outbreaks.5,6
WDGPH Strategic Commitment
Building Healthy Communities
We will work with communities to support the health and well-being of everyone.
Health Equity
Our programs and services use health equity principles to reduce or eliminate health differences in our communities.
Health Equity
Two population groups can be unintentionally negatively affected by the infection control measures Public Health recommends during a respiratory or enteric outbreak: the elderly residing in facilities and children attending daycare. It is important that with each recommendation Public Health makes the quality-of-life impact for elderly residents living in a facility is considered. This becomes increasingly important for residents in facilities which have difficulty controlling and ending outbreaks. Public Health must be available to consult daily with families and facilities on scheduled social activities and balance recommendations associated with the risk of disease transmission with the impact on quality of life.
Similarly, daycares provide an essential service for parents and a stimulating environment for children to encourage healthy growth and development. Recommendations for outbreak control must weigh the risks of increased child illness with the benefits of the outing, activity or play materials on the children’s healthy growth and development.
Appendices
NONE
References
- Ontario Public Health Standards. [cited 2016 Jan 16] Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/ophs_2008.pdf
- Ontario. Ministry of Health and Long-Term Care. A guide to the control of respiratory infection outbreaks in long-term care homes. Toronto, ON: Queen’s Printer for Ontario; 2015. Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/flu/docs/resp_infectn_ctrl_guide_ltc_2015_en.pdf
- Ontario. Ministry of Health and Long-Term Care. A guide to the control of gastroenteritis outbreaks in long-term care homes. Toronto, ON: Queen’s Printer for Ontario; 2015. Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/guidance/gd_control_gastroenteritis_outbreaks.pdf
- Update on influenza antiviral drug treatment and prophylaxis for the 2015-2016 season: update. Can J Infect Dis Med Microbiol. Available from: https://www.ammi.ca/guidelines/
- Ontario. Ministry of Health and Long-Term Care. Institutional/facility outbreak prevention and control protocol. Toronto, ON: Queen’s Printer for Ontario; 2015. Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/institutional_facility_outbreak.pdf
- Ontario. Ministry of Health and Long-Term Care. Infection prevention and control in licensed day nurseries protocol. Toronto, ON: Queen’s Printer for Ontario; 2008. Available from: http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/infection_prevention_nurseries.pdf